Breast Cancer Care in the U.S. in 2026: Understanding Today’s Treatment Landscape
Breast cancer care in the United States continues to develop in 2026, influenced by ongoing research, improved diagnostic tools, and more individualized care planning. Treatment strategies are increasingly structured around patient-specific factors, offering clearer frameworks for decision-making. Reviewing these changes can help patients better understand how care options are evaluated and discussed today.

The landscape of breast cancer care in the United States continues to evolve with advancing medical technologies, refined treatment protocols, and improved patient support systems. As we move through 2026, patients and their families benefit from a more comprehensive understanding of available treatment options, risk factors, and the decision-making processes that guide personalized care plans.
Early Signs That Often Prompt Medical Evaluation
Recognizing potential warning signs plays a crucial role in early detection and successful treatment outcomes. Common symptoms that prompt individuals to seek medical evaluation include lumps or thickening in breast tissue, changes in breast size or shape, skin dimpling or puckering, nipple discharge or inversion, and persistent breast or underarm pain. Changes in breast texture, unexplained swelling, or the appearance of orange-peel-like skin texture also warrant medical attention. Healthcare providers emphasize that while these symptoms can indicate various conditions, prompt evaluation ensures proper diagnosis and timely intervention when necessary.
Factors Associated with Breast Cancer Risk
Multiple factors contribute to breast cancer risk, ranging from genetic predisposition to lifestyle influences. Age remains the most significant risk factor, with incidence rates increasing after age 50. Family history, particularly in first-degree relatives, and genetic mutations such as BRCA1 and BRCA2 significantly elevate risk levels. Hormonal factors including early menstruation, late menopause, and hormone replacement therapy also play important roles. Lifestyle factors such as alcohol consumption, obesity, physical inactivity, and reproductive history including age at first pregnancy and breastfeeding duration influence overall risk assessment. Environmental exposures and previous radiation treatments to the chest area further contribute to individual risk profiles.
Main Therapeutic Pathways Physicians May Assess in 2026 and How Treatment Decisions Are Shaped
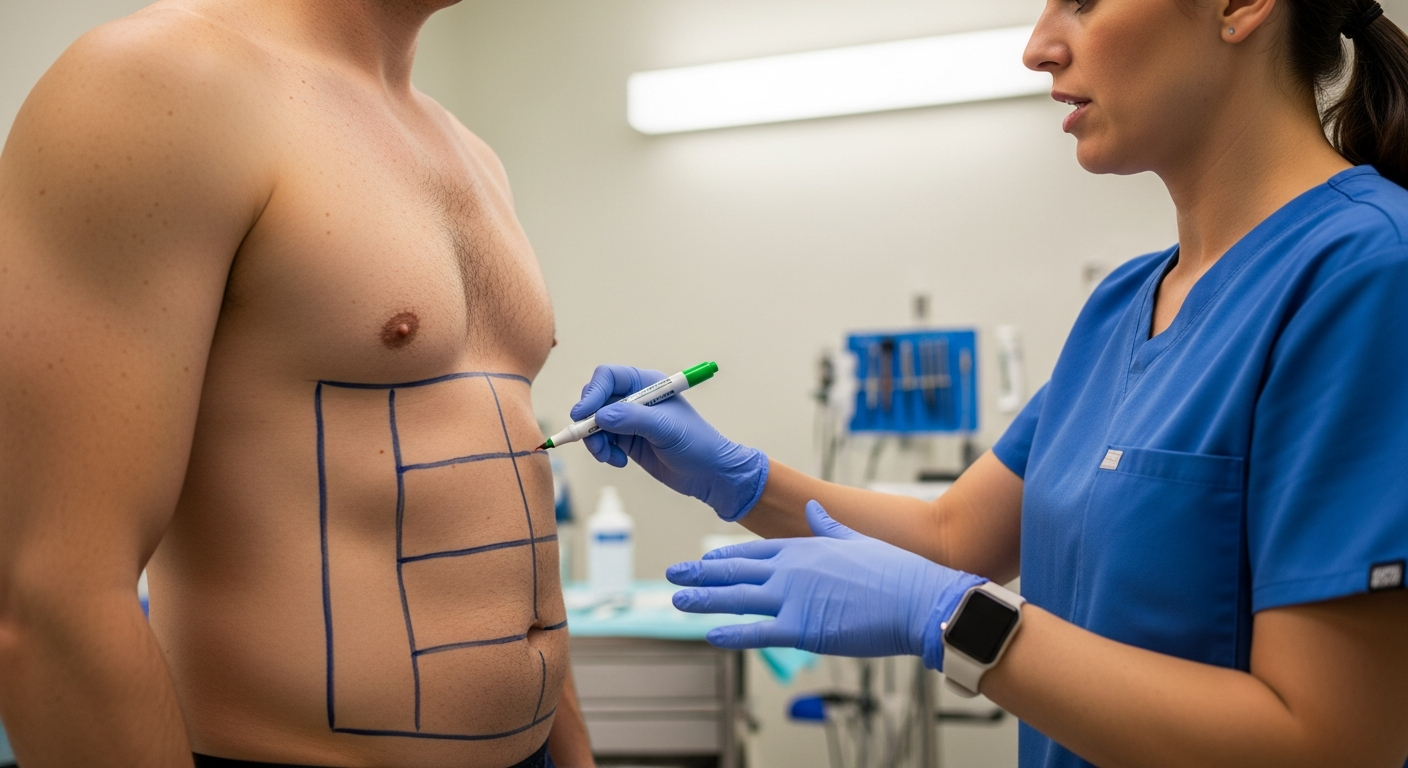
Contemporary breast cancer treatment involves multiple therapeutic approaches tailored to individual patient needs and tumor characteristics. Surgery remains a cornerstone of treatment, with options ranging from lumpectomy to mastectomy depending on tumor size, location, and patient preferences. Chemotherapy protocols have become increasingly targeted, with oncologists selecting specific drug combinations based on tumor biology and genetic markers. Radiation therapy techniques have advanced significantly, offering more precise targeting while minimizing damage to surrounding healthy tissue. Hormone therapy proves particularly effective for hormone receptor-positive cancers, while targeted therapies address specific molecular pathways. Immunotherapy represents an emerging frontier, harnessing the body’s immune system to combat cancer cells. Treatment decisions incorporate tumor staging, molecular profiling, patient age, overall health status, and personal preferences to create individualized care plans.
Questions Many Patients Consider Before Beginning Care in the U.S.
Patients facing breast cancer diagnosis often grapple with numerous concerns before initiating treatment. Common questions include understanding the specific type and stage of their cancer, exploring all available treatment options, and learning about potential side effects and long-term impacts. Many patients inquire about second opinions, clinical trial opportunities, and the expected timeline for various treatment phases. Financial considerations, including insurance coverage and out-of-pocket expenses, frequently influence treatment decisions. Patients also seek information about fertility preservation options, particularly younger individuals planning future pregnancies. Quality of life concerns, work accommodations, and family impact considerations play significant roles in treatment planning discussions.
| Treatment Category | Average Cost Range | Key Providers/Centers |
|---|---|---|
| Initial Consultation & Diagnosis | $3,000 - $8,000 | Mayo Clinic, Johns Hopkins, Memorial Sloan Kettering |
| Surgery (Lumpectomy) | $15,000 - $35,000 | Cleveland Clinic, MD Anderson, Cedars-Sinai |
| Surgery (Mastectomy) | $25,000 - $50,000 | Dana-Farber, Mass General Brigham, UCSF |
| Chemotherapy (per cycle) | $8,000 - $15,000 | Kaiser Permanente, NYU Langone, Stanford Medicine |
| Radiation Therapy (complete course) | $20,000 - $40,000 | UCLA Health, Mount Sinai, Duke University Hospital |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
How Treatment Strategies for Breast Cancer Are Developing Across the U.S. and What Patients Should Know
Breast cancer treatment strategies continue evolving through ongoing research, clinical trials, and technological innovations across American medical centers. Precision medicine approaches increasingly guide treatment selection, with genetic testing helping identify optimal therapeutic pathways for individual patients. Multidisciplinary care teams now standard practice, bringing together oncologists, surgeons, radiologists, pathologists, and support specialists to coordinate comprehensive treatment plans. Telemedicine integration has expanded access to specialized care, particularly benefiting patients in rural or underserved areas. Clinical trial participation offers access to cutting-edge treatments while contributing to medical advancement. Patient advocacy programs and support services have become integral components of cancer care, addressing emotional, financial, and practical needs throughout the treatment journey.
Navigating breast cancer treatment in 2026 requires understanding the complex interplay of medical, personal, and financial factors that influence care decisions. With continued advances in treatment options, early detection methods, and supportive care services, patients have access to more personalized and effective treatment strategies than ever before. The emphasis on patient-centered care ensures that individual preferences, values, and circumstances guide treatment planning alongside medical considerations.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.